The eradication of malaria has been given a boost this week following a grant of more than £1 Million from Japan’s Global Health Innovative Technology (GHIT) Fund to facilitate the production, testing and validation trials of the world’s first ever saliva-based rapid diagnostic test (RDT).
This significant round of funding, secured earlier this month by the University of Florida, will aid final product development to complete the commercialisation process of the RDT, by medical technology start-up Erada Technology Alliance.
South Africa-based Erada Technology Alliance, in collaboration with international partners CellFree Sciences, Frontier Institute, Johns Hopkins University and Oasis Diagnostics, aims to launch the diagnostic tool in 2021, with field trials being rolled out in the Democratic Republic of Congo or Uganda in Q2, 2020.
Easy to use, the tool incorporates a simple device for the collection of saliva and is designed so that healthcare professionals, teachers and parents can implement the procedure quickly and simply.
Conventional blood-based tests are more invasive, have to be administered by clinicians and encroach upon the ‘blood taboos’ which exist in many countries. Skin-prick tests moreover are often stressful for children and indeed their parents.
The grant for this pioneering innovation has come at a time when the World Health Organisation’s (WHO) Strategic Advisory Group on malaria eradication is calling for more innovative tools to overcome the existing suite of diagnostic tests.
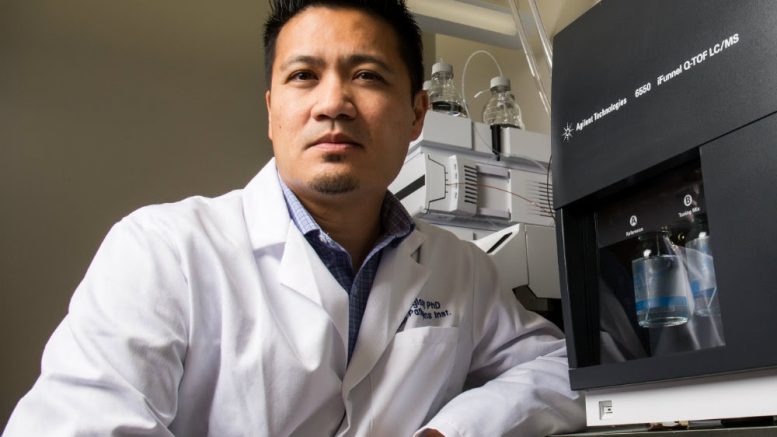
The new diagnostic is to be marketed around the world under the brand name SALVA! and uses technology developed out of research carried out by Professor Rhoel Dinglasan at the University of Florida.
Dr Dinglasan and his team identified a new P. falciparum protein biomarker (PSSP17) in saliva that could replace presently used parasite markers like the Plasmodium histidine-rich protein-2 (HRP-2), which have become increasingly ineffective due to a growing prevalence of parasite mutations and inherent difficulties and shortcomings of blood-based RDTs.
The Global Health Innovative Technology (GHIT) Fund, headquartered in Japan, is an international public-private partnership between the Government of Japan, 16 pharmaceutical and diagnostics companies, the Bill & Melinda Gates Foundation, the Wellcome Trust and United Nations Development Programme.
GHIT facilitates international partnerships that bring R&D innovation, investment, and leadership to the global fight against infectious diseases such as malaria, tuberculosis, and neglected tropical diseases in the developing world.
Ms. Catherine K. Ohura, CEO of GHIT said: “Through this investment, we are thrilled to have extended our portfolio in our quest to use technology to save lives across the globe. We have now invested more than 17 Billion Yen to causes that will help prevent the deaths of millions of children and adults.
“Rapid diagnostic tests are crucial in curtailing malaria, the reason why we decided to invest in this innovative project and partnership led by the University of Florida.”
Erada Technology founder, Dr Benji Pretorius, said: “This vitally important investment paves the way for the eradication of malaria. The deadly disease, indeed one that I was fortunate to recover from myself, snatches the lives of more than 435,000 globally each year. Many of whom are children under the age of five.
“That this swiftly follows a foundation grant from De Beers Group has significantly aided both the work that we and our collaborative partners are striving to achieve, and the fight to eradicate malaria on a global scale. We can now push on with field trials and commercialisation which we hope to complete by World Malaria Day in April 2020.”
GHIT’s six-figure backing of the commercial development of SALVA! will cover three essential objectives:
- Design and small-scale production of 2,000 SALVA! kits, which contains a saliva-collection device and a lateral flow immunoassay cassette.
- Quality-assured medical device production conditions of heat-stable, high-affinity recombinant humanized monoclonal antibodies for capture and detection of PSSP17 on a lateral flow test.
- Thorough testing and validation of the commercial SALVA! test in the Democratic Republic of Congo (DRC), a priority malaria endemic country, or Uganda.
During these studies, the acceptability, usability, sensitivity and reliability of SALVA! will be compared to the most sensitive molecular laboratory tests used in malaria detection.
The overall outcome of the project is to fulfil all the criteria for obtaining CE marking and subsequent WHO prequalification of the SALVA! kit.
ERADA’s saliva test detects a unique biomarker from female parasites circulating in an infected human who is asymptomatic (not displaying symptoms) but is carrying the parasite and likely to come down with malaria within a week.
Early subclinical and asymptomatic disease detection, in addition to detection of carriers – individuals who carry a specific parasite lifecycle component without falling ill from it – is crucial to malaria eradication. Carriers are the reservoirs which lead to infection of mosquitoes and transmission of the disease.
Detecting the presence of the parasite before symptoms appear can save lives because malaria visible disease only erupts a couple of days after the mosquito bite.
The SALVA! detection tool works by detecting a novel biomarker for Plasmodium falciparum parasites in saliva. In some areas of the world, the parasites have acquired a mutation and are therefore no longer detected by current blood-based tests. But ERADA’s saliva test detects an essential protein the parasite needs for survival, which should avoid the problem of influence from the mutation and keep the test effective long-term.