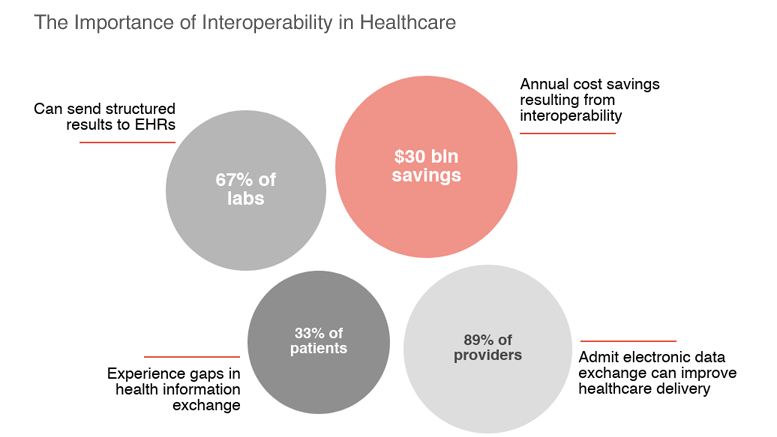
Healthcare professionals agree that consistent data exchange between medical technology systems and software solutions (the phenomenon is also known as interoperability) and further data analysis is crucial to shifting from episodic to continuous patient care. Semantic interoperability can also eliminate the virtual and physical barriers to healthcare knowledge sharing within organizations and help hospitals identify bottlenecks and manage assets more effectively.
Current interoperability initiatives, however, are undermined by outdated EHR systems, the lack of health IT standardization and information blocking.
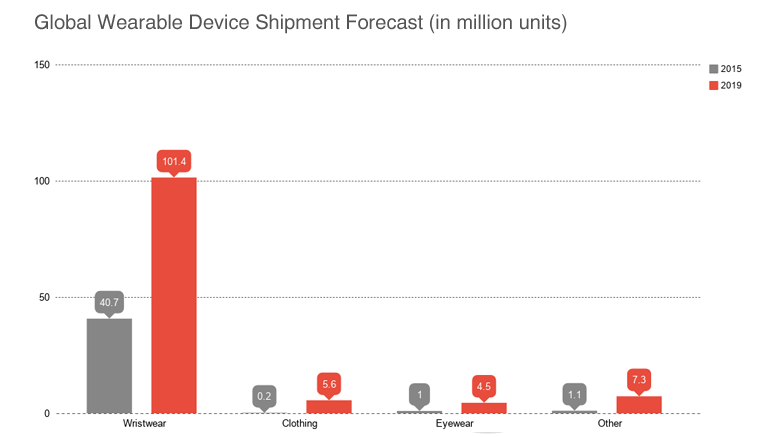
Could wearables — bracelets, personal heart monitors, smart glasses, medical dispensers and other devices with built-in connectivity — possibly promote the development of a data-centric approach to healthcare delivery?
Wearable Technology: an Effective Way to Achieve Healthcare Interoperability
In recent years, we’ve seen more wearables move from the wellness segment to real-time patient monitoring — largely due to advances in IoT technology, the diminishing price of sensors and greater availability of open-source APIs, frameworks and libraries enabling fast and cost-effective software product development.
Some examples of such wearable diagnostic and assistive devices include the cancer-monitoring iTBra patches which detect metabolic changes in heat that correlate to breast tumor cellular activity, the L’Oreal UV sensor which measures UV exposure and the Owlet baby monitoring sock which tracks oxygen levels, heart rate and sleep.
Medical wearables’ superpower comes from the ability to collect valuable information; provided sensor data is analyzed and acted upon, healthcare professionals could achieve greater transparency in day-to-day operations and improve patient outcomes.
Examples of Healthcare Interoperability Challenges That Can Be Solved with the Wearable Technology
Identity Management
Accurate patient identification and matching to EHRs is crucial to healthcare delivery and coordination, both within a particular medical institution and nationwide. In the USA alone almost 200 thousand deaths occur each year because of medical errors, and 58% of those result from identity errors.
The UK-based Heartlands Hospital which serves over half a million people annually was one of the first healthcare organizations to leverage the power of wearables for improved patient identity management. The hospital addressed Zebra Technologies to increase the efficiency of their operating theatres; the proposed solution featured printed wristbands with RFID tags which contained patient digital images and healthcare records and software with image processing capabilities. During the pre-surgery checks, the system required clinicians to scan patients’ wristbands using PDAs, thus eliminating misidentifications and providing up-to-date information on a patient’s well-being. The implementation of the RFID-based solution helped the hospital reduce identity errors to zero and perform one extra surgery daily — which, among other things, generated an unplanned income of over $ 300 thousand annually.
RFID- and barcode-based wearable solutions can also support other medical procedures that require patient identity verification, such as bedside medication delivery and blood transfusions, and be integrated into healthcare security solutions to enable role-based access to patient data.
Knowledge Management
Wearable devices collect vast amounts of relevant data which can help healthcare professionals discover correlations between medical conditions and manage them more effectively.
Cardiovascular care, for instance, is already benefiting from analyzing the data gathered via wearable fitness trackers: besides heart rate, the tiny devices allow physicians to track patients’ physical activity and daily calorie intake.
Wearable computers — including the infamous Google Glass — provide quick access to patient data stored stored online or in healthcare databases, enable remote collaboration between healthcare organizations and could potentially streamline healthcare training.
The Google Augmented Reality glass, for example, has been successfully used by cardiac surgeons to navigate CT scans in hands-free mode during coronary revascularization. Back in 2014, a British surgeon also used the AR gadget to broadcast a cancer surgery to over three thousand medical students from 116 countries.
Barriers to Wearables’ Implementation in Healthcare
- Data accuracy & reproducibility. Wearable devices generate measurable data on patient behavior and well-being, including glucose levels, heart rate and other vitals. However, many gadgets are not FDA-approved and therefore might provide inaccurate sensor readings. Furthermore, real-time data processing and visualization are essential to implementing medical wearables on a large scale: even a 2-3 second lag can seriously affect the performance of healthcare systems which make use of sensor data and prevent physicians from drawing immediate conclusions from it. Therefore smart healthcare solutions development is often preceded by the so-called Discovery Stage aimed at choosing the right technology for the project and feature set optimization, which translates into additional (and often unexpected!) expenses for healthcare providers.
- Growing diversity of medical wearable solutions. From basic printed tags to pills enhanced with sensors which allow physicians to track patient medication adherence, medical wearables exist in a variety of forms. They aggregate different types of data and may use different connectivity technologies, which again brings us back to the question of the development and implementation of unified interoperability standards.
- Questionable impact on patient outcomes. According to a study published by the Cedars-Sinai hospital earlier this year, the use of wearable technology for remote patient monitoring, for example, has limited impact on clinical outcomes — largely due to the inconsistency of the available data and immaturity of the wearable technology itself. Wearables, however, proved useful in fostering healthy habits and improving self-care.
Researchers believe that findings from wearable monitors could potentially help healthcare professionals develop personalized treatment plans and anticipate the need of intervention before symptoms of a certain disease occur. FDA shares the enthusiasm, too: with the introduction of their Digital Health Precertification program in late 2017, we can expect more innovate medical wearables to be released to the market. Last but not least, the medical gadgets unveiled during 2018’s CES were positively different from earlier offerings and featured complex back-end systems facilitating data aggregation and analysis.
Are you ready for the change?





