An Artificial Intelligence algorithm which can identify future hip fracture patients is being used by hospitals to provide better care and reduce costs.
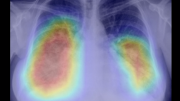
The program looks through thousands of existing CT scans already held by NHS Trusts, quickly identifies vertebral fragility fractures (VFFs) and returns the scan to the hospital with the fractures clearly ’flagged up’ for further investigation. In doing so, it also frees up valuable time for specialist doctors to use their expertise and skills where they are needed most.
Funded by the National Institute for Health Research Invention for Innovation programme, the process has been developed by the University of Manchester and Central Manchester Hospitals NHS Foundation Trust, in collaboration with Optasia Medical Ltd with input from the Royal Osteoporosis Society.
Fractures due to osteoporosis affect half of all women and 1 in 5 men aged over 50. By 2025, treatment of fractures is estimated to cost the UK over £5.5 billion1.
“Vertebral fractures are the most common osteoporotic fracture and are the most predictive of subsequent hip fractures. The cost to both the patient and the NHS of further fractures can be avoided if we design systems that are alert to a patient’s first vertebral fracture”, says Richard Evans, Chief Executive Officer, Society of Radiographers.
According to the Royal Osteoporosis Society more than 55% of hip fracture patients have evidence of a prior vertebral fracture. The average cost of a hip fracture to an NHS hospital was found in a 2015 study2 to be £16,302 in the first two years.
Using the new technology, Optasia Medical has already carried out two successful pilots in collaboration with Nottingham University Hospitals NHS Trust and Bradford Teaching Hospitals NHS Trust, referring a total of 1,432 previously undiagnosed patients for further assessment and treatment.
“This is how AI delivers real world benefits to both patients and healthcare budgets”, said Optasia Medical’s Chief Executive Shawn Luetchens.
“The fractures are found in existing CT scans which have been commissioned for another investigation but happen to image the spine, so there are no new imaging costs which helps hospitals make the most of NHS resources.
“Once the algorithm has done the spadework by finding the fractures and flagging them up, the results are verified by a consultant radiologist before being returned to the hospital.
“This is a very efficient use of a consultant radiologist’s expertise at a time when the UK has a shortage of them3”.
Once at-risk osteoporosis patients have been identified they can be placed on a drug regime and given lifestyle assistance both of which help to strengthen bone density.
“Patients have the opportunity to lead a healthier, more protected and active life. And over the course of a few years, hospitals will start to see a big reduction in the number of elderly patients coming back into hospital with costly hip fractures”, said Mr Luetchens: “So far we have processed just a few patients from two hospitals and we are already looking at potential surgical cost savings to the NHS of more than £10 million”.
Artificial Intelligence applications for radiology and other healthcare technologies are being developed at pace around the world.
The project in Manchester is one of the first in the UK to deliver an application with real-world benefits that can be accessed by hospitals to provide more effective care for patients and reduce costs.
- Osteoporosis in the European Union: a compendium of country-specific reports. Arch Osteoporos. 2013; 8(1-2): 137 (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3880492/)
- NHS hospital costs after hip fracture were found in a 2015 study by researchers from the University of Oxford and the MRC Lifecourse Epidemiology Unit in Southampton to be an average of £16,302 in the first two years following the incident.
- The Royal College of Radiologists say that the vacancy rate for consultant posts has increased from 9% to 10% in two years. https://www.personneltoday.com/hr/radiologist-shortage-make-service-collapse/