For most, pregnancy and childbirth should be a positive and happy experience. But on those occasions when things do go wrong, the effects can be devastating for families. The Health and Social Care Committee report on the safety of maternity services in England, published recently, highlights how there has been progress in recent years but that a culture of blame and staff shortages have prevented some services performing to their potential. As the report describes ‘too often families are not provided with the appropriate, timely and compassionate support they deserve’.
The state of affairs
Major concerns were recently raised at Sheffield Teaching Hospitals Foundation Trust. After an unannounced inspection from the CQC, the maternity units were downgraded from ‘outstanding’ to ‘inadequate’.
What many of these investigations highlight is the need to improve safety and listen more to patients within maternity services. The fundamentals of delivering quality healthcare services are ‘safe, effective, and experience’ as stated by NHS England – pillars which can be upheld by harnessing and responding to patient feedback about their experiences. Patient views are often considered secondary to clinical opinions, but in reality, patients are very good at identifying safety issues such as medication errors or missed tests. Patients aren’t simply a recipient of care, but an active participant in it, and are well placed to observe changes in their care that aren’t right.
Last year’s Ockenden Review, an independent inquiry into Shrewsbury and Telford Hospital Trust’s maternity services, recommended a number of improvements. These included better listening to patients within maternity services and enhancing safety. The Health and Social Care Committee report also identified that services need to deliver on listening to their patients; ‘families must be confident that their voices are heard and that lessons have been learnt to prevent the tragedy they have endured being repeated’.
Patient Insights – Case in point
Analysis of trends and variation in patient experience have recently helped to show health and care providers how their departments and services are perceived, but most importantly, how they can take action, by understanding what patients think, say and value about their experience of care.
Drawing on relevant publicly published patient comments, PEP Health has revealed insights identifying deteriorating care and key patient concerns months in advance of the Sheffield Teaching Hospital’s maternity services’ CQC inspection.
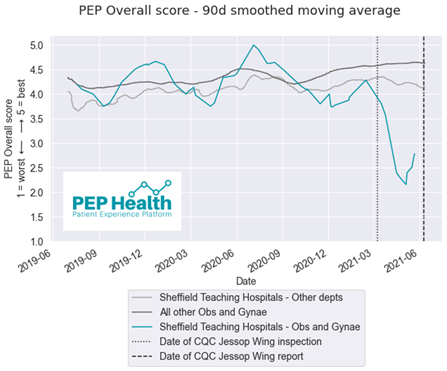
Their analysis of comments made by mothers and families being cared for from June 2019 to June 2021 revealed three key insights. Firstly, that patient experience in maternity is far below the national average. Secondly, that the remaining hospital services at Sheffield Teaching Hospitals NHS Foundation Trust are not experiencing the same deterioration in care as the maternity unit. Thirdly, and most importantly, their data shows patient experience steadily declining from as early as summer 2020, months ahead of the CQC inspection on 9 March 2021.
Data shows that other departments at the trust were performing well in terms of patient experience with the average score being 4.2/5.0, when Obstetrics and Gynaecology received a concerning score of 2.1, as seen in the graph above. Most interestingly, the data shows that the rest of the hospital has not seen a decline in experience of care, whereas the maternity unit had reported decreases from as early as the summer of 2020. The CQC inspection was not carried out until March 2021, and while the outcomes from CQC and PEP Health are aligned, the patient comments gathered over the year before the inspection explain why the CQC verdict was reached. Even more crucially, it provides actionable insight into how that verdict could have been avoided.
Sheffield Teaching Hospitals’ maternity services could have anticipated their CQC rating before it was made by listening to and responding to patient comments on their care. By using comments from patients that were published publicly such as on social media, PEP Health is able to harness the real patient voice and share actionable insights with care providers. The steady decline in the patient data highlighted could have acted as an early warning system for poor patient experience. This knowledge could then have been used to improve the service, while also fulfilling the Maternity Services Report‘s expectations of ensuring “voices are heard”.
The Patient Safety Strategy from NHS England outlines that “better incident reporting and response could save an extra 160 lives and £13.5 million”. Patients can be a part of this incident reporting, and in fact they already are, organically on their preferred channels. By using their comments and feedback on social media, organisations can turn them into actionable insight and minimise patient safety concerns.
What makes a healthcare system ‘good’?
A new approach is needed for how patients’ views are used as a force for good, to not only enable positive change but allow organisations to fix issues before they take hold. Using patient insights should go hand in hand with clinical effectiveness and patient safety, allowing for continuous improvement and supplementing the CQC’s quantitative methods.
PEP Health’s data analysis over the last four years shows that maternity provision has one of the highest levels of variation, with some trusts showing consistently high ratings while neighbouring trusts can have very low ratings. By using patient insights from across the system neighbouring NHS trusts and departments can learn from one another and improve.
In order for services to be safe, effective and responsive it goes without saying that providers must look at the patient story, to avoid stark consequences. It comes down to making use of early warning signs, of which patient insights can be a huge contributing factor.
Healthcare systems need to invest in safety, effectiveness, and experience in order to deliver quality care. Right now, the experience of care by patients lacks serious investment. Viewing the patient as an active participant in their care and understanding the potential impact their views can have on the quality of care given, can directly avoid situations like those at Sheffield from happening again.
Sheffield Teaching Hospitals confirmed they ‘wasted no time’ in addressing the issues that surfaced from the CQC inspection. This highlights that a more proactive and less reactive strategy is needed to help organisations futureproof against problems with patient experience. Getting an ‘outstanding’ CQC inspection is not the be all and end all, it’s about delivering better care to patients.
Undoubtedly, there is a needed culture change in the way that patient experience is considered, and indeed valued. The report outlines that this culture change can’t simply be legislated for, which may be true. However, if you make listening to your patients a core part of your strategy, it can become a part of your culture. It comes back to that all important point: “families must be confident that their voices are heard”. Really, it goes beyond just hearing, and really listening to inform future actions, so that patients receive the “appropriate, timely and compassionate support they deserve.”





