Avrim Fishkind, MD, General Manager, Psychiatry for SOC Telemed discusses the role of telepsychiatry, as a viable solution to today’s mental health crisis in prisons and jails
The inadequate treatment of mentally ill prisoners across the U.S. is at national crisis levels as evidenced by the special update on the mental health of incarcerated populations, published by Bureau of Justice Statistics in 2017. The report highlights a bleak reality: U.S. prisons and jails are to capacity with people experiencing mental health problems. Half of prison inmates and two-thirds of people in jails reported serious psychological distress or a history of mental health problems; and of these, only a third reporting serious psychological distress were receiving treatment.
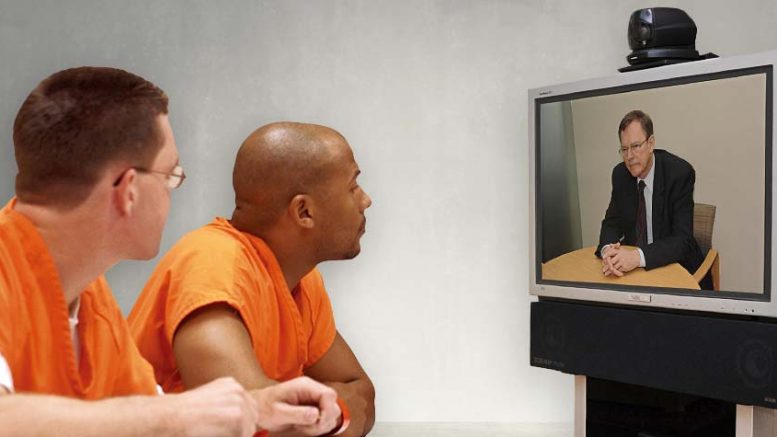
Correctional facilities in the U.S. are considered the largest provider of mental health services. Yet many prison systems struggle to provide adequate treatment, even after lawsuits and courts demand access to mental health care. Why? They lack the financial resources and the necessary mental health staff to provide treatment to everyone who needs it. This is not to say all is lost. Telemedicine, specifically telepsychiatry, can help improve access to mental health services for inmates.
By its very nature, telemedicine serves to connect healthcare providers with patients in need. Similarly, correctional systems are beginning to see how telemedicine can offer them a comprehensive telepsychiatry approach for cost savings, timely access to mental health care, and overall better health for both inmates and staff. Consider these leading benefits of using telemedicine in a correctional setting:
Improved Mental Health
Without mental health services in the community, many people with mental illness have run-ins with the law and end up in prisons ill-equipped to give them the care they need. Correctional facility staff may not be trained to handle the misbehavior, for example, in a manner that benefits these inmates and corrects the behavior. Sheriff’s deputies with little or no training in psychiatric care typically respond to misbehavior as they are trained — with force and isolation, both of which generally exacerbate mental illness. Conversely, a mental health professional is equipped with an assortment of care-oriented responses focused on improving behavior, managing the symptoms and encouraging recovery. Telemedicine brings this expertise in-facility, making timely and humane mental health treatment accessible to inmates.
Reduced Recidivism
Reports show that nearly 50% of people in state prisons with a mental illness were incarcerated for a nonviolent crime. Once in prison or jail, lack of treatment/medication and even the strict conditions typically cause substantial and rapid deterioration in their condition. It’s a destructive series of events: a person with mental illness is incarcerated for a small infraction; once in, their mental conditions worsen; this leads to behavioral and other issues that result in extended sentences. To make matters worse, when they get out, they’re ill-equipped to deal with life. The bottom line is that prison inmates who don’t receive the mental health care they need are more likely to cycle in and out of the criminal justice system. Appropriate and continuous mental health care is the key to breaking this cycle.
Promotes Staff & Public Safety
In the event of a serious mental crisis — with no mental health support on staff — most protocol calls for a prisoner transfer to a local hospital or appropriate medical facility. Such a scenario introduces the risk of prisoner escape or harm to the escorting officers and the hospital staff. The ability to bring trained medical professionals in-facility through technology negates the need for transport, thereby increasing staff and public safety.
Reduction in Costs
Lastly, are costs. Timely and continuous onsite mental health care leads to cost savings for correctional facilities in the form lower psychotropic medication costs, reduced transportation costs, reduced costs of recidivism, and improved medical care, which ultimately results in fewer medical complications, hospitalizations and lawsuits.
In all, telepsychiatry can serve as a critical component to solving the current mental health in our jail and prison systems. We must do more as a society to ensure psychiatric patients are diverted from correctional facilities to psychiatric hospitals, community-based mental health emergency centers, and crisis residential units, rather than costly, unproductive and harmful incarceration. In the meantime, telemedicine is the key to delivering appropriate, humane psychiatric care to inmates living with mental illness.
About Avrim Fishkind
Dr. Fishkind is a past president of the American Association for Emergency Psychiatry. He has designed multiple comprehensive psychiatric emergency programs including Psychiatric Emergency Rooms, 23-Hour Observation Units, Mobile Crisis Outreach Teams, Crisis Residential and Stabilization Units, Crisis Hotlines, and short-term Crisis Counseling Units. Dr. Fishkind has been employed in the delivery and development of psychiatric crisis services in many locations, including New York City, Austin, Texas, Houston, Texas, Washington, D.C, Portland, Oregon and most recently Omaha, Nebraska.