Patient safety and the prevention of harm is at the centre of all medical advances. And although millions of people receive successful cutting-edge treatments and medicines every year, when things go wrong it can result in serious suffering for the patients affected.
The long-term health effects when medical devices fail are highlighted in the IMMDS report First Do No Harm. This includes the thousands of women injured by pelvic mesh implants who have experienced life-changing complications, many of whom lost their mobility, relationships and jobs.
New medical device regulations designed to protect patients from incidents like these are due to come into force in 2025 and should be very much welcomed.
However, whilst strengthening the regulation of medical devices is an important step towards protecting patients, a tighter regulatory framework – if not constructed correctly – could unintentionally have the opposite result.
If it is too expensive or time-consuming to generate the amount of data required to meet the new regulations, patients may indirectly suffer. There is a risk that it could hinder the innovation of new products or reduce the availability of legacy devices.
Medical registries will play a pivotal role in striking a fine balance in this regard. Registries hold the key to essential information about the performance of devices and their impact on patient outcomes. This data will be critical in helping mitigate against the risk of the new regulations stifling innovation and reducing the availability of successful legacy devices.
The UK is well-placed in this respect as we already have arguably the best Joint Registry in the world, the NJR or National Joint Registry. And earlier this year, a registry for all implants was launched, the ORP, Outcomes and Registries Programme, delivered by NHS England. This is currently being rolled out across all hospitals.
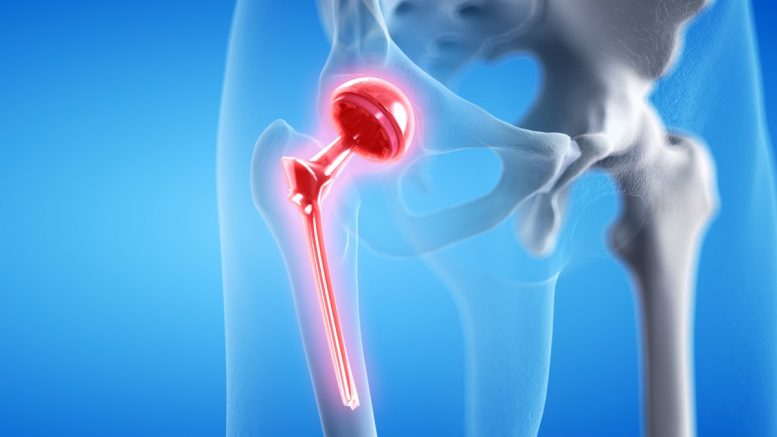
Registry data, along with other sources, is already used to benchmark all orthopaedic joint replacements through ODEP (the Orthopaedic Data Evaluation Panel). An independent panel of voluntary experts interpret the data to provide objective ratings on the performance of joint replacements. This helps hospitals and surgeons choose the very best and safest implants for patients.
The challenges of new medical device regulations
So while we strive to extend the scope of regulations to promote patient safety, we need to be careful not to discourage manufacturers from bringing ground-breaking new products to market. Or perhaps even see long successful products be withdrawn.
What we don’t want to see as an unintended consequence of the new framework, are fewer specialist options for clinicians. This could happen if the new MRHA regulations require greater volumes of data over much longer timescales.
If this is the case, manufacturers might find it difficult to secure approval for their smaller volume devices such as specialist joint replacements which could be removed from the market altogether.
In this case we may see patients not receiving the most appropriate implant, compromising the final functional outcome and with life-changing implications for the patient.
Take a specialist hip replacement that’s been available for 15 years for example. Under the new regulations manufacturers are likely to be required to collect extensive clinical data to ensure its continued availability to surgeons. But if they must pay vast sums to collect this data, it could result in the implant being withdrawn or becoming more expensive.
We then face a learning curve while surgeons learn how to use a new device, if the one they have previously performed many successful operations with, is no longer available.
It is a question of balance, as Tim Wilton, orthopaedic surgeon and Medical Director of the National Joint Registry explains. “Many of the steps to tighten the regulatory framework should be welcomed. However, it may be necessary to find a way to allow existing devices that work well to stay on the market, even when their usage may not be high enough to allow the manufacturer to justify the expense involved in going through the entire process repeatedly.”
Keeping the door open to innovation
If the regulations become too demanding, they may deter manufacturers from operating in the UK and lead them to focus on other countries instead. This would risk diminishing the UK’s status as an MedTech innovation hub.
Since we don’t want to close the door on innovation there is a tightrope to be walked.
Registries will be an instrumental part of that balancing act as they can provide the evidence needed for regulators within the new legislative landscape.
This is because, unlike a database which is simply a repository for data, a registry is a system which collects and monitors data contemporaneously that is then analysed regularly by medical professionals to evaluate outcomes.
In principle, a registry can collect data on every medical procedure. Each time a surgeon places a new device in a patient, those details are recorded.
Whilst nobody disputes the reliability of controlled clinical trials, registries are generally cheaper and more comprehensive. They nearly always provide reliable information more quickly, as the cohorts of patients are often so much bigger. Data is collected from all surgeons using the device and not just the design surgeon as is often the case with a trial.
Registries are much more cost effective for manufacturers to contribute to, rather than commission their own trials, which will encourage innovation as well as keeping successful devices in the market.
Consultant orthopaedic surgeon, John Skinner, explains why this is important. “We will always need manufacturers to develop new implants to solve complex individual situations such as when, a patient’s anatomy has changed from the standard situation, or has been damaged and needs complicated revision surgery.”
As the UK navigates the new medica device regulations and regulatory framework, it is crucial we prioritise both patient safety and the best treatment options. Withdrawing successful products from the market, or stifling innovation, is not the way to improve patient care.
Medical registries will play a pivotal role in getting this right, providing evidence for both new and established devices. By leveraging the data and insights from registries, the UK can offer the best treatment options available and continue to be a hub of medical innovation. This way, we can improve patient outcomes without compromising on safety.
About the author
Mr Keith Tucker FRCS is Chairman of the Orthopaedic Data Evaluation Panel (ODEP) and the Beyond Compliance Advisory Group. He explores these views further in ‘Medical device regulations: a step forward for patient safety or a step backwards for innovation?’