Chris Yeowart, Director at Wellbeing Software, discusses four specific areas that can help ease the NHS backlog while maintaining focus on COVID-19 efforts
A new report published by the Health Foundation has found that there were 4.7 million fewer people referred for routine hospital care between January and August 2020 due to elective services either being cancelled or postponed as a result of the pandemic.
Members of The Royal College of Surgeons also warned of a “tsunami” of cancelled routine operations as the NHS copes with rising numbers of coronavirus patients. The situation is equally difficult for patients with life-threatening illnesses such as cancer. Recent studies suggest a 25% backlog in referrals due to COVID-19 could result in 181 additional lives lost, with curable diseases becoming terminal after waiting for treatment.
To minimise the impact of the pandemic and reduce the backlog in routine services, hospitals and NHS Trusts need to be able to maximise available resources while adhering to social distancing measures. So how can we beat the build-up without jeopardising national COVID-19 efforts? I believe the answer lies in four key areas: shared resources in radiology, integrating diagnostic services, moving towards a virtual model, and connecting the dots with electronic health records.
Shared resources in radiology
Radiology departments play an essential role in the diagnostic process and as a result operate at the intersection of a vast array of healthcare services. This means they need to work faster and smarter. However, a consequence of fewer radiologists and growing demands during the pandemic has left services stretched beyond capacity, resulting in reporting delays.
With social distancing measures in place and a greater emphasis on remote working, radiologists need to be able to access reports, even when they are away from the original scan site.
This is why delivering an integrated approach to information-sharing within and between different NHS services should be a priority. By bringing data together, radiologists across the country can have access to the same centralised patient record at all times. This helps clinicians share resource and access scans remotely to make faster and better-informed decisions and enable patients to move more seamlessly between services.
Integrating diagnostic services
It is clear that organisational change is required to improve patient outcomes, not only during the pandemic but also to ensure illnesses are diagnosed efficiently. To do this, hospitals and laboratories need to make adjustments to working practices in order to increase diagnostic capacity and speed up the process between testing and results. We can do this by optimising resources across lab medicine, pathology, and radiology.
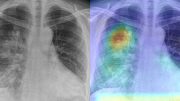
Providing a single integrated view of diagnostic tests, images, reports, and results could help to streamline that process, which is critical to making a prompt diagnosis and enabling the rapid commencement of treatment. Better access to data also offers an opportunity to deploy business intelligence and clinical workflow optimisation tools to provide better visibility of cases, and management of resources. Artificial intelligence algorithms can also be introduced, to support workload prioritisation and enable even greater efficiencies in the diagnostic process.
Moving towards a virtual model
One significant consequence of the pandemic has been the accelerated adoption of digital solutions to support the national response to coronavirus. Remote hospital outpatient appointments have been shown to keep patients safe by reducing unnecessary travel, with the number of remote consultations starting at around 200 per day but rapidly increasing in their thousands.
NHS services have worked incredibly hard to deliver the same in-person experience for patients through virtual mediums. The adoption of electronic patient communication platforms, video consultations, and remote assessments has shifted care from the physical to the virtual and we can now understand how to receive and deliver effective care remotely.
The transition to virtual appointments was happening before COVID-19, but the process has been vastly sped up, and while there is some inconsistency, most Trusts are fully or partially prepared to deliver remote services. However, it is important that we do not neglect regulations or clinical standards during the pandemic, and tools such as electronic consent enable clinicians to conduct the necessary risk assessments while minimising hospital visits or time spent in a waiting room.
Connecting the dots in electronic health records
Clinicians need to have quick access to patient records to ensure swift diagnosis and to create appropriate treatment plans. However, specialities can often exist in silos despite the fact they share comparable features. These disparate systems can impact continuity of care and cannot adequately support the needs of multi-disciplinary teams (MDT) especially during a crisis.
To address the challenges associated with fragmented care and the increasing pressure to deliver elective services, it’s important that hospitals and NHS Trusts have access to singular electronic patient records which can be accessed across multiple departments or sites. This gives clinicians a richer picture of the patient to ensure treatments are delivered safely and in a timely way.
The health pandemic has highlighted more than ever the crucial role that digital technology plays in healthcare, and the challenges presented by the COVID-19 outbreak have acted as an opportunity to profoundly change the way healthcare is delivered. The pressing need to adopt technology solutions is a chance to make significant progress in embedding digital technologies into clinical care across the NHS.