A 2018 survey conducted by the UK agency Medicines Discovery Catapult found that 80% of SMEs (small to medium sized biotechs) found accessing biosamples from the national health service ‘unexpectedly difficult with the result that 75% imported samples from abroad’.
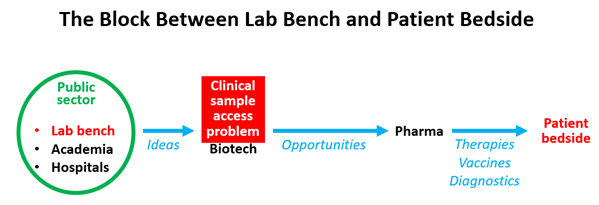
It turns out that this problem is not just in the UK. Biotech companies everywhere in the world have great difficulty accessing high quality patient biosamples to support their research and development. At the root of the problem is the simple fact that patient samples most often originate in a healthcare setting in the public sector. Biotechnology companies are in the private sector and therefore have reduced access.
About Hospital Biobanks
Hospital biobanks generally exist in teaching hospitals and academic centres, they are publicly funded and are established for the purpose of supporting research in associated universities and institutes. They require dedicated staff and expensive equipment—such as liquid nitrogen freezers—so the start-up and maintenance costs are considerable. While the start-up phase may be funded by research grants, it is harder to obtain research funding for the on-going maintenance costs of these unglamourous yet essential core facilities. So, many biobanks survive on funding provided by their own institution. A typical hospital biobank may have 2-3 staff working extremely hard within a very tight budget to provide professionally curated clinical samples for in-house researchers.
One way in which biobanks can develop an independent income stream is to charge a fee for the provision of patient biosamples. However, this must be approached with caution as it is illegal to make a profit from the sale of human tissue in many countries. So, biobanks are allowed to charge a carefully calculated cost-recovery fee.
Access to a biobank’s samples is decided by scientific and ethical committees that are populated by various institutional members (scientists, clinicians, administrators, ethicists), with the frequent addition of a patient representative. These committees judge the merits of each application for samples, and they operate according to institutional policies.
One issue that sometimes reduces the likelihood that biosamples will be provided to industry is the concern that some patients may not want their samples to be used by commercial organisations that make a profit from them. Whether patients react in this way is very much dependent on how matters are presented to them and whether or not the societal value of industry research is emphasised.
In many cases these biobanks are open to applications from industry, in theory at least. Biobanks of different specialities can be found in various national and regional biobank directories, but unfortunately their level of interest in working with industry is often obscure. So, we have the problem that useful biobanks are hard to find.
Why small Biotechs and Big Pharma are very different
Sample access problems are bigger for smaller, younger biotech companies than for established pharma companies. For one thing, these pharma companies will have had many years to develop networks of hospitals supplying samples. Additionally, the fact that pharma companies conduct clinical trials gives them access to hospitals, doctors and patients. Many large pharma companies have teams of dedicated clinical sample procurement staff and their own in-house biobanks, which often dwarf those found in typical hospital biobanks.
In contrast, a small biotech company, particularly a start-up, has none of these advantages and certainly cannot afford to have staff dedicated to sample procurement.
Obtaining BioSamples ‘From Abroad’
In general, the easiest way for biotech companies to obtain samples is to get them from a commercial broker. These companies have the sole focus of providing clinical samples for industry, and naturally they are driven by the need to make a profit.
Brokers generally find it difficult to obtain their samples from hospitals and biobanks in western Europe, where ethical concerns about the sale of human tissue are prevalent. Some countries in eastern Europe and parts of Asia provide a more reliable source. The USA is one industrialised country where brokers are much more accepted, with many US hospital biobanks being willing to supply brokers. The majority of brokers are based in the USA, and many of these have sample procurement operations that extend across global networks.
Scientifically-speaking, the main disadvantage of using a broker is that sample provenance may be lacking (brokers tend not to reveal their sources for business reasons) and along with this there may be uncertainty about the quality of the samples and hence the reliability of resulting research.
Better Solutions
So, what can be done to provide industry, and particularly small biotech companies, with the high-quality, reliable samples they need? This is important because all of us, as patients (past, present or future), depend on the drugs, diagnostics and vaccines that biotech companies make possible. The answer is that some practices need to be encouraged, while others need to be discouraged.
- Encouraging Best Practice
It must surely be best practice for any researcher to obtain biosamples direct from source, that is, directly from the hospital biobank that collected the sample from the patient. In this way, they can have the most confidence that samples and data have been collected professionally. So biotechs should ideally obtain their samples direct from hospital biobanks.
To encourage this, we need to make it easier for biotechs and hospital biobanks to find each other. Biotechs can search a number of biobank directories to find suitable partners, but this is often a difficult approach. Many of the biobanks listed may not be open to working with industry, or may give companies a low priority. Use of biobank directories often results in a lot of disappointing false leads.
One initiative that offers a solution is the online platform, Biosample Hub. This international platform is dedicated to bringing biotechs and academic/hospital biobanks together, and its use is restricted to these two groups. It includes a directory of biobank and biotech members, a directory of sample requests and social networking features. The only reason for biobanks to be on the platform is to supply industry, so the problem of false leads is minimised. One other key aspect of the platform is that it is not-for-profit, so this overcomes the ethical concerns of many biobanks.
Another way to encourage this is to make it more attractive for hospital biobanks to work with industry. In other words, there need to be more and bigger incentives. The problem is that for many hospital biobanks, local academic researchers get top priority, other academic researchers get second priority, leaving industry at the end of the queue. This is natural, because these biobanks are established as institutional initiatives, with the purpose of serving their own institution. The focus of academic biobanks is very much on research productivity as measured by publication impact, and unfortunately industry, for reasons of intellectual property, faces restrictions about how much work it can publish and when.
The incentive of funding is certainly the most viable option for getting hospital biobanks to work with industry. Biobanks need funding and often operate on shoestring budgets. Much has been written on the subject of biobank sustainability, especially financial sustainability. One approach is for biobanks to charge industry a cost-recovery fee for its biosamples and also to charge a fee from additional sample processing services, such as cutting sections and extracting DNA. This approach seems to be especially well understood by French biobanks, who use the term valorisation for the process of adding and yielding value from their samples. Almost half of the biobanks that have joined Biosample Hub are French and most offer additional sample processing services. All French hospital biobanks are certified according to the French norm NF S96-900 which must also make them more attractive to industry.
Another approach is to make external grant funding of biobanks conditional on service to industry. This could be aided by making it mandatory for funded biobanks to make their sample access policies public, by requiring annual reports on sample distribution and perhaps even having industry representatives on sample access committees. Patient representatives are well accepted, so why not industry representatives?
An example of the kind of support needed is provided by the following statement from the UK Medical Research Council: ‘The development of new drug therapies, and diagnostic and screening tests, to the point where they can be made sufficiently widely available to benefit human health, is crucially dependent on commercial involvement. Therefore, access by the commercial sector to samples of human material collected in the course of MRC-funded research should be facilitated, where this is consistent with our mission.’
- Discouraging The Use of BioSamples That Lack Provenance
New regulations are likely to have a major impact on how biotech companies source their clinical samples. An example is provided by the new European regulation governing manufacture of in vitro diagnostic devices, which comes into force on the 26th May 2022. To demonstrate conformity, makers of IVDs must show that the biospecimens used to validate their devices have undergone acceptable pre-analytic processing. This will require the sourcing of samples from biobanks that are certified to meet specific quality management standards. As a result, diagnostics companies will need to obtain samples from known sources that provide full provenance information.
This need for provenance information will put pressure on commercial brokers to change their business practices and reveal the source of their samples. One way in which brokers may mitigate this is by using binding contracts with both the provider and the requestor of samples, to prevent them from interacting independently of the broker. Of course, not all companies or biobanks will be comfortable with such restrictions.
There are technological solutions that can be used to ensure the reliability of provenance information of samples and use of these will be beneficial. The use of blockchain is one example. This digital technology allows tracking of the transfer of biospecimens from the patient donor to the researcher in a secure, transparent and ethical manner, with all transactions documented in an incorruptible shared digital ledger.
The time seems ripe for a major change in the way clinical samples are sourced by industry and by smaller biotech companies in particular. Now more than ever, as a result of the pandemic, the general public understands the importance of biotech and pharma companies.
ABOUT THE AUTHOR
Robert Hewitt, MB BS, PhD, is the founder of Biosample Hub, a new platform that connects Biotech companies looking for samples, with Biobanks that have ethically sourced samples available.

