Adherence to medication has been a longstanding issue for healthcare globally for many years. According to the World Health Organisation (WHO) research, it is estimated that 50% of patients with chronic illness do not take medications as prescribed. Poor medical adherence to prescribed medicine increases patient morbidity, increased hospitalisations and pressures put on healthcare services. Further, poor adherence to medication is estimated to incur costs of approximately $100 billion per year globally, which is approximately 1.5% of global healthcare spending. This translates to an eye-watering £2bn in NHS spending in the UK. This is a huge amount of money that could and should be better resourced.
Poor medication adherence is defined as any situation where a patient is not taking their medications as prescribed by their physicians. This may include forgetting to fill prescriptions, taking medications at the wrong time of day, taking them incorrectly, or not at all. In fact, most people have been, or are currently culprits without even knowing it. Education and access to information is clearly part of the problem.
However, it’s important to be aware that taking medications and using medical devices can be complicated. Reading labels and instructions can be daunting, especially if you are newly diagnosed, overwhelmed by a new condition or are feeling unwell. In addition, there are a many different medical devices that deliver medication, such as inhalers for the treatment of asthma, meaning if patients choose to search for their devices online, they run the risk of following incorrect guidance and misusing their device, leading to poor deposition of the medication.
If around 50% of patients with chronic illnesses are not taking medications as prescribed, this is extremely problematic for several reasons. Most importantly, if these patients are not taking their medication for their condition then despite their best efforts and good intentions of going to the doctor, their health is being compromised. Secondly, this can mean medical resources are being wasted and a financial burden placed unnecessarily on our healthcare system.
Technology and digital therapeutics can provide personalised medical support to meet the specific needs of patients. Impact on patient outcomes, caused by poor medical adherence can be reduced through technologies such as validated and approved digital therapeutics and virtual patient consultations. In fact, widespread technology implementation will save the NHS billions.
For example, exclusively showing patients the relevant information for their health requirements, such as demonstration videos of how to use their specific asthma inhaler, as opposed to a number of different inhalers, the margin for errors in use is reduced by 80%. In addition patients are not overwhelmed with irrelevant information and can instead focus on learning the specifics related to their health condition.
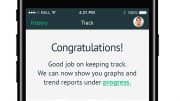
Evidence-based digital therapeutics is an example of where to start addressing the issue. It increases efficiency and fosters patient knowledge and in turn confidence for accurate and effective self-management. Similarly, reporting mechanisms and mobile health apps demonstrates how technology can future proof administering care and contribute to the recovery of the NHS post-pandemic.
Ensuring patients are equipped with the correct information at the time when they need it the most guarantees that they are prepared and set up for success. Personalised medicine requires personalised education and this is an area in which digital therapeutics can excel. In doing so, technology can improve medical adherence and save the NHS millions.
Article by Dr Simon Bourne, Chief Executive Officer at my mhealth