Delivering patient-initiated follow-up (PIFU) is a major new change to outpatient services laid out in NHS England’s Operational Planning Guidance and is almost certainly going to be a major component of the Elective Recovery Plan.
With two thirds of all hospital appointments taken up with often unnecessary follow-up reviews, patients can find these appointments inconvenient in terms of travel, financial costs and time out of work. These unnecessary appointments also place an exceptional burden on clinical and administrative staff. PIFU aims to reduce this by empowering patients to be partners in the decision about when to have their next follow-up appointment.
The target in December, which the majority of NHS trusts missed, was to have 1.5% of all outpatient attendances on a PIFU pathway with the service to be trialled in at least five major outpatient specialties. Against a backdrop of winter pressures, and a burnt-out workforce, is it even possible for the NHS to deliver on what are almost certainly going to be tougher targets in the Elective Recovery Plan?
Simplifying PIFU through digital
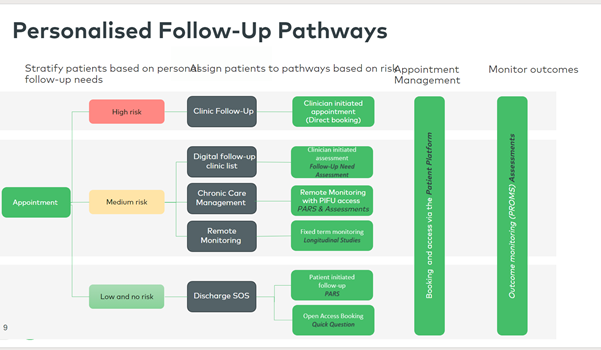
While getting any version of PIFU in place is a starting point, to achieve maximum benefit we need to review entire pathways and integrate PIFU at the most optimum point alongside things like digital assessments. PIFU is sometimes viewed as a project in isolation and digital projects are not viewed as part of a wider transformation of the pathway.
There is also inconsistency around whether PIFU is really digital or not. Many trusts believe they already have a digital form of PIFU in place because they are using spreadsheets or non-integrated lists to manage the pathway. But this doesn’t solve the issue of being able to automate the service and reduce the time spent on admin. As a result, opportunities to maximise the number of patients suitable for PIFU are missed and the benefits to staff are overlooked.
PIFU, incorporated as part of a digital pathway, gives trusts the ability to tailor the messaging, length of service, number of booking requests and provision of additional monitoring requirements. Forward thinking trusts are already scaling PIFU digitally. One is about to rollout digital PIFU in 30 specialities by tailoring solutions to specific pathway requirements. This has enabled those trusts to make a dramatic impact on the way they deliver care and communicate with their patients, giving a better experience of care overall.
The current challenges we face in scaling PIFU
One of the barriers to delivering PIFU at scale is the present lack of evidence of just how effective it can be, therefore providing an incentive to implement it. This is in part because there is large variation across NHS trusts about the definition of what PIFU actually is.
A clear, consistent definition of PIFU is essential to determine how many people are suitable for it and to understand and measure the real benefits. PIFU is categorised into four groups, ordered from lowest risk to highest risk:
- Open Access Booking
- See On Symptom (SoS)
- See On Need (SoN)
- SoN Patient initiated chronic care management
- Clinically initiated – remote follow up management
- Remote monitoring
For example, while some trusts are seeing a 35% reduction in their follow-up waiting lists, in reality they are only using it right at the end of the pathway to ‘discharge to SoS PIFU’. This limits the benefits that patients could have by attending fewer appointments earlier on in their treatment and giving time back to both patients and staff.
The right patients for PIFU
One of the key areas where PIFU can be most effective is with long-term health conditions or pain management. In this instance patients are assigned to a pathway, complete periodic digital assessments and given control to book their own appointment. They receive real time information about their condition, and depending on the result, can request an appointment. Clinicians can still initiate appointments based on their review of the digital assessments through clinician-initiated follow-ups (CIFU).
The other option is to integrate a digital See on Symptom PIFU list where patients are assigned to a pathway and given control to book appointments should their symptoms worsen. This solution helps negate concerns providers may have about patients no longer being monitored or managed when discharged.
PIFU should exist as part of the pathway – helping to optimise it and give patients the opportunity to take control of their wellbeing in a streamlined way. By consistently using PIFU in the management of long-term conditions, in conjunction with other digital tools such as remote monitoring and longitudinal studies, large cohorts of patients can be easily identified and placed on the pathway.
Mitigating risk to patients
What about the risk to patients when they are no longer seen for their usual outpatient appointments at 6, 9 or 12 months?
We need to have effective communication about the changes to all patients so that they understand they are being given a choice. One idea currently being examined is whether patients could be automatically scheduled in for a six-month follow-up and then given the ability to choose, if they feel it’s necessary, whether they have a 3, 9 or 12-month review. For the 15 million people living with a long-term health condition, this could be a game changer.
If this approach can be applied consistently, and if patients understand this is the case, it will free up consultants to see the next person on the waiting list. It would also mitigate any risk by providing a way to monitor patients so that they don’t fall through the gaps.
Looking at PIFU as one part of the digital pathway puzzle also misses the opportunity to actually deliver personalised appointments and prevent wasted time for both patient and clinician.
This is where the true value lies – in being able to personalise what people need and ensuring PIFU is not a one size fits all. Ultimately, we need to ensure the people who are put on a PIFU pathway are most suited to it.
Personalised outpatients and unlocking growing waiting lists
Using digital to optimise pathways allows for far greater impact than introducing PIFU alone. If we start to view healthcare through the lens of the patient and redesign it in a way that works for them, we can improve our outpatient follow-up offer.
Digital delivery of PIFU gives the opportunity for trusts to deliver healthcare in a way that empowers patients, reduces waste and frees up time. This inevitably reduces the backlog and improves the overall experience for patients and clinicians. Whether that’s through patients requesting a blood test slot instead of just turning up, by supporting discharge or through virtual wards, where patients have the control to book their own appointments should their symptoms flare up.
With PIFU targets looming we need to consider how to improve the patient experience and help trusts think differently about the way they meet these targets. If PIFU isn’t working then let’s start talking about personalised follow ups instead.
By Tom Whicher, CEO DrDoctor

