Offering precision targeted radiation treatment, healthcare professionals are often surprised to learn that the technology behind Gamma Knife treatment is not a new concept, having been in mainstream treatment use for the past 50 years. University College London Hospital (ULCH) is a pioneer in stereotactic treatment, the method having first been developed by two British scientists in 1908 working at the same hospital; its Queen Square Radiosurgery Centre (QSRC) is now a leading international Centre of Excellence for Stereotactic Radiosurgery.
GammaKnife has been used to treat a wide range of brain tumours from metastatic tumours to benign brain lesions and neurovascular conditions. As outcomes and survival rates improve for cancer care, QSRC has witnessed considerable growth in the volume of metastatic cases referred for Gammaknife treatment. Post covid, QSRC is seeing many more patients with multiple metastases and this is where GammaKnife compared to other platforms can offer particularly effective treatment.
During the last 15 years, GK became a recognised treatment for the small to medium-size acoustic neuromas and other skullbase benign tumours like meningiomas, where open surgery would generally carry a significant risk of morbidity and cranial nerves deficits.
The paradigm of management has changed from the classical ‘wait and see’ policy followed by surgery, to a more proactive approach of offering Gamma Knife treatment for small tumours, in the early stages of their diagnosis, in order to preserve, as much as possible, the function of the affected cranial nerves (eg the facial nerve and the hearing for the acoustic neuromas).
Growing usage of GammaKnife Technology
Other areas where GammaKnife is increasingly recognised as an alternative treatment option is for functional neurological conditions such as tremor, epilepsy and some psychiatric disorders. Leading Gamma Knife centres around the world are routinely providing GammaKnife thalamotomy treatment for patients with essential tremor and this is a service QSRC is keen to offer to the NHS patients, although government funding still needs to be secured.
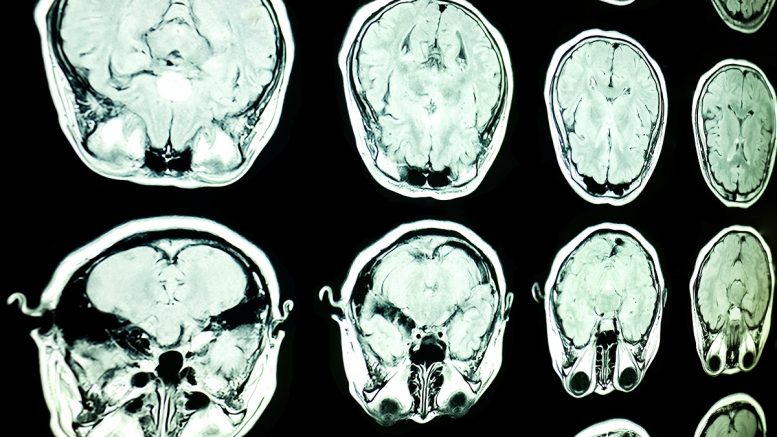
Initially used for ArterioVenous Malformation (AVM) treatment, with classic catheter angiography for vascular target delineation, the development of Gamma Knife as a brain tumour treatment has come a long way with the advancement of imaging such as MRI and CT scanning. With the progress of more detailed structural imaging, and incremental improvements in Gamma Knife technology, the treatment technique has become an established and proven treatment modality with a track record of success.
As surgery progresses towards less invasive options, further advancements in imaging and mapping technologies allowing higher levels of precision are fast developing. We have seen this with the introduction of the new Vantage frame which, being made of fibre glass instead of metal, allows for superior imaging by significantly reducing any frame-induced artefacts and the potential magnetic fields induced heating. Software developments are enhancing imaging techniques for improved treatment planning and mapping saving time and further improving treatment accuracy.
The technology is always evolving. QSRC has recently introduced pre-plan or pre-treatment scanning for rapidly progressive metastatic cases where the tumours maybe spreading more aggressively than we would like. Pre-planning scanning, particularly, with the new Vantage Frame, allows the use of enhanced diagnostic imaging (for example on a 3T MRI) to better identify the overall volume and target to treat more accurately and successfully. This is proving an exciting quality development introduced at QSRC this year.
Since the the Gamma Knife upgrade to the Icon model at QSCR in 2018, we have been able to extend the classical volume-related limitation for the lesions amenable to treatment. By using fractionated treatment with mask fixation or adaptative staged treatments, we can now offer Gamma Knife treatment for larger lesions previously considered too large for a ‘single fraction’ of GammaKnife treatment and still surgically inoperable.
Treatment with mask fixation together with the use of the new more ‘patient friendly’ Vantage frame have improved patients’ comfort during procedure allowing them to have a personal choice of their ‘journey’ through this procedure.
The increasing availability of immunotherapy and targeted molecular therapies for cancers has definitely improved the prognosis of patients with brain metastatic disease. This allows Gamma Knife stereotactic radiosurgery to be offered in addition to these therapies in cases previously considered too far advanced for radiosurgery to be worthwhile. Now Gamma Knife treatment is frequently offered to patients with a high number of small brain metastases, before or during their extracranial systemic cancer treatment resulting in a really good treatment response to brain metastatic disease.
Indications for Gamma Knife radiosurgery are expected to extend to ‘nodular’ lepto-meningeal disease and other advanced forms previously reserved for palliative whole brain radiotherapy which tends to impair and/or reduce cognitive brain function. Now with Gamma Knife we can give patients much better quality and longer life with less brain impairment.
In some international Centres, and in the US particularly, there is much work taking place using Gamma Knife to treat behavioural disorders. The disorders examined include obsessive compulsive disorder, anxiety disorders, , separation anxiety, and various mood disorders. This is an exciting development in the use of Gamma Knife treatment and we will continue to watch this space carefully to better understand whether Gammaknife can improve treatment of mental health conditions.
By Mr Neil Kitchen, Medical Director at QSRC and Mr Cornel Tancu, Clinical Fellow, QSRC