From hearing an Olympic gold medallist to frontline stories of digital adoption in health and social care, Joined-Up Health and Care 2018 provided lessons for urgently needed change.
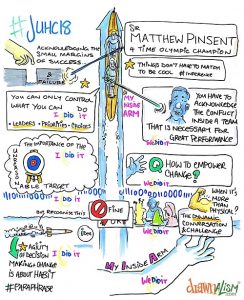
“Control the controllable,” said four-time Olympic gold medallist Sir Matthew Pinsent during his keynote address to delegates at the fifth annual Joined-Up Health and Care conference.
Sir Matthew might not have navigated a large-scale hospital IT deployment, or the task of integrating data across a myriad of organisations and care boundaries. But his ideas still resonated with the hundreds of individuals gathered in Birmingham at The Belfry, eager to inform their own prescriptions for keeping digital healthcare transformation afloat, efficient and effective.
Parallels of pressure in Olympic success
Set against ever rising tides of pressure faced by NHS and care services in the UK, the conference heard how Britain’s world leading rowers had faced comparable challenges as their own targets had continued to elevate, with substantially higher demands placed on teams at every Olympic Games.
“We knew that if all we did was to carry on doing what we were doing, we would end up between two and four seconds behind the mark,” said Sir Matthew, who gave an emotive address on the teamwork, leadership and transformation continuously needed to win every four years.
“The number of variables that go into that performance are astronomical. You try and persuade yourself that you are in control of all of them, but you aren’t.”
The challenge: “How do we empower people in our system, in our crew, to say ‘we know we must change, how are we going to do it?’ You have got to come up with metrics about how you are going to show improvement.”
Incremental and ongoing improvement in the NHS
Ahead of the conference, Downing Street pledged an additional £20bn in NHS funding by 2023. But with growing demands inevitably set to accompany new funds, the need for continuous, incremental and measured improvement, echoed throughout the conference after Sir Matthew sat down.
“Activity is going up across the UK,” said Deloitte director Mike Hay who, reflecting on findings from the last five years, pointed to a 21% rise in outpatient demand in the UK and the fact that “A&E demand is continuously going up.”
“We haven’t got the numbers we need to deliver services,” he added, referencing falling bed numbers and an increase in staff that was not “the rise that is needed.” The NHS was a “hot system” with high levels of bed utilisation. This “really tough” environment meant “every little thing you do matters, especially when the system is under pressure,” said Hay.
Staff motivation was a key factor. “If we can reduce staff absence by a third, we would save around £500m in temporary staff,” he said. And the NHS needed to ensure its technology becomes “fully used”, with complete adoption a priority.
Managing complex delivery
Dr Graham Evans, chief information and technology officer at North Tees and Hartlepool NHS Foundation Trust, told the conference he had created a “handbook of complex delivery” on realising that one didn’t already exist.
With trust ambitions to reach the globally renowned highest digital maturity rating of HIMSS EMRAM stage 7 within three years, there were already key lessons to be shared from the organisation’s deployment of InterSystems TrakCare as its new electronic patient record, and from its digital transformation mission as part of a wider region.
Key components of success for Evans rested around managing “people, process and technology,” but it was also “about starting with the basics, communicating the direction you want to take.” Evans told the floor: “We make everyone in the organisation aware of what we have done, why we are doing it and what the benefits are going to be.”
“When you deliver technology there will be things you haven’t event dreamt of,” he said. “You need to deal with the unexpected, things will go wrong on that journey, and you need to have a root and branch review of things that go wrong to understand the real reasons and the facts.”
As the first English edition trust, Evans insisted that “TrakCare was a good decision”. “It has not been an easy journey developing something from scratch, you do take risks. But we are on a journey together, it is a partnership between ourselves and our key vendor InterSystems.”
Encouraging colleagues in the room to also think beyond their own organisation, he said: “You need to be tenacious in the agenda and have a ruthless determination to deliver.”
The hospital and beyond
InterSystems vice president Don Woodlock gave global examples of how InterSystems technology is being used to “unify the health multiverse” – thinking far beyond the acute environment. This included the NHS Coordinate My Care service, which had used InterSystems HealthShare platform to build an online care plan for urgent and end of life care patients, changing the patient experience, preventing inappropriate hospital admissions and informing actions for emergency and out-of-hours responders across London. On the other side of the Atlantic in New York City, he recalled how Healthix, the country’s largest health information exchange, had connected information for more than 600 organisations and 16 million patients.
Such scale would now be of value for the UK’s vision. Malcolm Senior, NHS Digital’s programme director for integrating care, told the event: “What we are trying to do with national interoperability is to build things at scale. That really does mean everybody pulling together. There is no room on that boat for passengers.”
Philip Graham, digital programme lead at Healthier Lancashire and South Cumbria, gave a powerful example of local and national working together to this end. Supported by HealthShare, he detailed how a project in his locality is helping to progress a national programme around transforming the flow of information for the care and wellbeing of children for the first years of their life. Part of the task was to deliver 70,000 e-redbooks by March 2019. “The key to the programme is to know where every child is, how healthy they are and what we are doing about it. This needs to permeate everything – it doesn’t just work in Lancashire or London, we have to interoperate information wherever a child might have a vaccination, or a development check. That’s not just healthcare – that is schools and social care as well.”
Not just about Lancashire, Graham explained how the HL7 FHIR standard based project with InterSystems was enabling events management and feeding information to the national level where appropriate – to systems like the Spine, and Citizen Identity. As well as being able to empower parents with reminders for vaccinations, or provide information to fathers and grandparents when appropriate, this was in part about “national fail-safes.” “One of the big reasons we are doing this is that children went missing, and they came to great harm because of it,” he said. The project would also reduce the need for health workers to manually input information into a child’s Redbook, with information able to automatically flow from different systems capturing it.
Mike Green, chief clinical information officer at South Devon and Torbay NHS Foundation Trust, also told delegates of his experience of using HealthShare to break down silos of information within the hospital and to start to connect the health and care landscape in South Devon.
“Information sharing isn’t enough,” Green told delegates. “We have also got to look at workflow. And if you really want to go digital you have to look at data capture. I shadowed one of my colleagues in an emergency department using their paperless system. It took him about 10 minutes to assess the patient and about 30 minutes to do the data entry and referral.” Green observed that though the emergency department system was forcing the clinician to do their job “properly”, it was nevertheless intrusive to the delivery of healthcare. “We need to find ways of supporting workflow and data capture in a meaningful way,” he said.
Engagement – what’s in it for me?
With many of his own colleagues lacking interest and enthusiasm for IT, Green spoke of the limits of the attention span of clinicians for technology. But effective engagement was still seen as vital to avoid informaticians developing a “digital version of the paper process.”
And engagement needed to be a continual process, the conference heard. In an address on using the electronic patient record to improve patient safety, Dr Iain Mackenzie, physician executive at InterSystems, said “it is absolutely vital to ensure maximum clinical engagement at all levels – not just your thought leaders.” Taking engagement to the next level, he also remarked “training is forever…not just for your go-live event.”
Yet when it came to ongoing engagement in reality, Jason Hess, executive vice president for strategy at KLAS Research revealed that his organisation had found that fewer than 7% of providers were getting feedback from their clinicians on satisfaction of their electronic medical records.
There were rules for effective engagement, delegates were told. Dr Yossi Cohen, a practising NHS clinician, and physician executive at InterSystems, looked beyond clinical engagement. He told delegates successful patient engagement meant encouraging “not easily impressed” patients to actually use systems. Providers and suppliers were often fixated on savings and care improvements as reasons to use technology. Cohen said: “Patients don’t care about that.”
“When a patient is going to log into a patient portal they think ‘what is in it for me’,” he said. “If you are going to engage a patient you need to look at the project through their eyes – what they are going to achieve, not what you are going to achieve.” This, added Cohen, required understanding the motivations of different patient cohorts, and engaging with each cohort differently.
From customers, for customers
JUHC 2018 offered significant opportunity to share best practice in the same year that both InterSystems turned 40 and of the 70th birthday of the NHS. For InterSystems vice president of international business Steve Garrington, it was an opportunity to talk to customers directly. And it was successful customers, delivering against challenging pressures, that made the event worthwhile.
“I walk into many of my customers’ environments day in day out, and I am struck by the operational challenges,” said Mark Palmer, country manager for UK & Ireland. “The NHS sees 1 million patients every 36 hours and delivers 10 million procedures a year. That is a huge operational challenge, and when you are trying to deliver digital technology to improve the delivery of care, it is like changing the engines while you are flying the plane.” JUHC offered an opportunity to listen to NHS users on how they were achieving the “very, very difficult”, task that Palmer described.

