What has been standard in other industries for many years is becoming increasingly an issue in healthcare – simulation and modeling in the virtual world. By using so-called virtual twins, valuable insights can be gained to advance medicine, research and patient care.
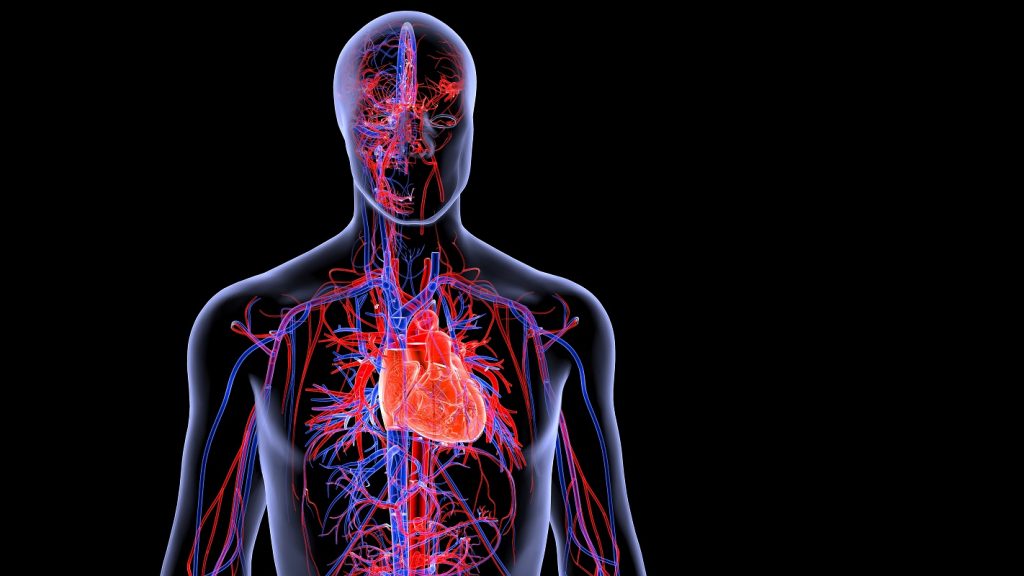
The use of simulation and 3D modeling for developing and testing new products has already proven its worth in many industries. In the automotive industry, for example, physical crash tests are rarely carried out, as these are nowadays primarily performed in a virtual environment. In medicine, however, it is still common practice to work with 2D images that do not provide a complete picture of the patient’s situation. Since the data is now available in digital form, transforming the current standard to 3D will enable what works well in other industries: virtual twins. This approach – the digital mapping of real objects and processes – makes it possible, for example, to virtually analyse body parts, individual organs or the entire human body. Moreover, by training the models with real patient data, results can be simulated under the same conditions as the real counterpart.
One medical discipline that can particularly benefit from virtual twins is cardiology. Figures from The British heart foundation show that Heart and circulatory diseases cause a quarter of all deaths in the UK, that’s more than 160,000 deaths each year – an average of 460 deaths each day or one every three minutes in the UK. There are also around 7.6 million people living with a heart or circulatory disease in the UK. Modern treatment methods and prevention are essential pillars for improving patient care. To adapt the virtual twin technology to the human body, Dassault Systèmes launched the Living Heart Project in 2014.
The Living Heart Project
The Living Heart Project aims to make the virtual twin of the human heart a reality. To this end, more than 100 institutions from research, industry, medical professions, and regulatory authorities have joined forces. In cooperation with Dassault Systèmes, they developed the first realistic 3D simulation of a complete beating heart using the SIMULIA software solution.
Science and research have been dealing with the complex conditions of the human heart for decades and thus contribute significantly to the success of the Living Heart Project. The interaction with other organs, drugs and treatment methods is of particular interest. In this way, the researchers are making a valuable contribution to being able to map a fully virtual construction of the heart. However, given the complexity of (congenital) heart defects and how they interact with medical devices and replacement tissue, this still requires intensive research.
The clinical environment is also intricately linked to the Living Heart Project. The challenge here is to research innovative treatment methods cost-effectively while meeting high regulatory requirements for safety. Companies from the medical technology sector – such as manufacturers of medical device components, already use the model during the development phase. They can test new applications and devices directly on the Living Heart model through simulations. The findings from the virtual test labs reduce expensive and time-consuming prototype construction, and animal testing can be reduced. Unlike animal models, the virtual heart can incorporate clinical data to represent a human heart more accurately over time as it is used; this enables faster development and approval, contributing to faster time-to-market for new medical devices. At the same time, company feedback helps further develop the model.
Where are we seeing this practice used today?
Today, personalised heart models are used to support clinical treatments, for example, in operations to correct severe heart defects in new-borns. Here, many virtual surgeries can be performed under the physician’s guidance to determine the best approach.
Medical students, hospital staff, and even patients also benefit from the Living Heart – for example, the virtual twin of the heart can be used in education and training in the healthcare sector to train surgical procedures in the virtual world. In addition, development cycles and test series could be accelerated and optimised thanks to simulation. For example, it is possible to better adapt artificial heart valves to the disease conditions of groups or individual patients with the help of the virtual heart – many of the time-consuming and controversial physical tests on animals or specially made laboratory models are thus no longer necessary.
Next Step: The virtual human body
What is still being researched today may already contribute to raising patient care and the development of drugs or medical technology to a new level tomorrow. Dassault Systèmes is, therefore, already working with partners on other organs, such as the Living Lung and the Living Brain. The Living Brain, for example, is currently being used to research neuronal disorders such as epilepsy. Here, brain activities can also be simulated from individual patient data, helping to understand this disease, predict seizures or classify seizure types.
The virtual models of these complex organs are already so advanced that it is possible to think one step further – combining the various individual models and thus simulating the entire human body. Such use of the virtual twin paves the way for further advancing the development of personalised medicine. Every patient, therefore, has the chance to receive treatment tailored to their body, genes, and metabolism.
By Steve Levine, Sr. Director of Virtual Human Modeling – Dassault Systèmes