The NHSX Data Saves Lives strategy is one that the medical imaging sector should pay close attention to, writes Sectra’s Chris Scarisbrick.
There has been a lot of reaction to June’s NHSX led ‘Data Saves Lives’ strategy from suppliers in the electronic patient record space. The draft document should be commended for its focus on standards and on overcoming some of the big obstacles still faced in the health and care around data access and availability.
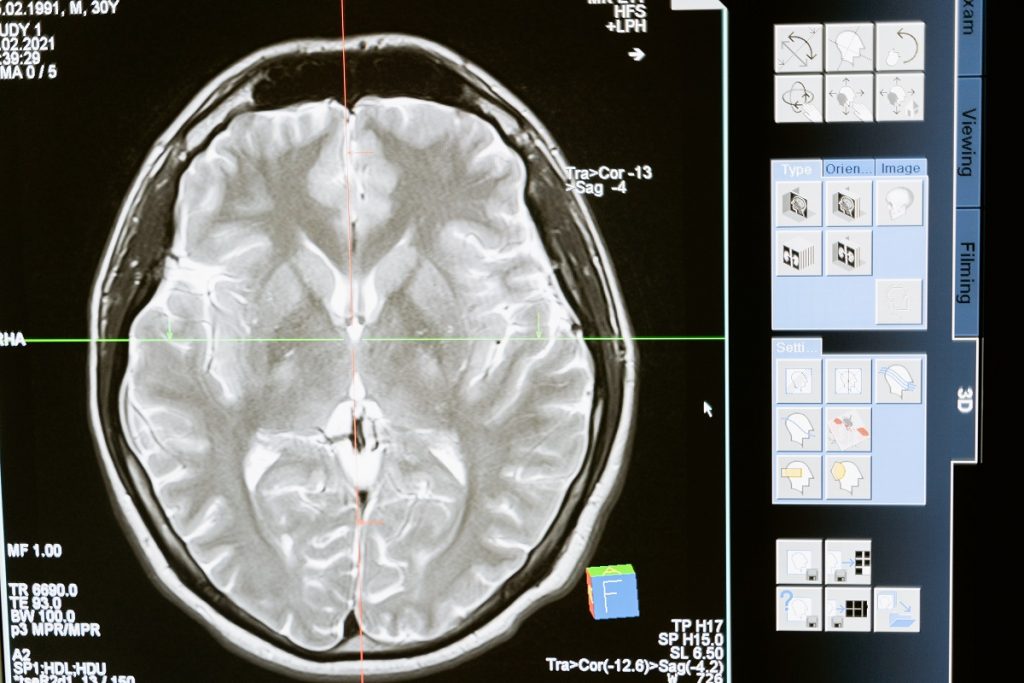
But it is important to remember that data is about more than numbers and words – textual information contained in records. If we are to make the most of emerging strategic direction on data, we also need to think about how it could apply to one of the biggest sources of data in the health service: imaging.
Radiology was one of the first diagnostic disciplines in the NHS to become digital – moving away from light boxes and film 20 years ago. Other diagnostic disciplines are now following in its footsteps. For example, many large scale digital pathology programmes that cover populations of millions of people are moving from slides and microscopes to high resolution digital images – where images can be instantly shared with the right specialists.
Disciplines including medical photography, microbiology, cardiology, dermatology and many other diagnostic ‘ologies’, collectively create a wealth of cradle to grave imaging data, but in many cases siloed approaches have persisted, sometimes impacting directly on patient care.
The challenges of indiscoverable imaging data
The pressure placed on radiology to keep up with demand and report in a timely way has never been greater. Yet we know that a lack of access to data in clinical settings means that many chest x-rays, CT scans and other diagnostic tests are repeated unnecessarily. In the case of radiology that means wasted resource as images are re-acquired, before being re-reported by a radiologist. But it also means bringing that patient back in for their scan, and unnecessarily irradiating the patient.
Systems like the Image Exchange Portal have helped in part to address the challenge – which is typically used in the NHS to share anywhere up to 35-40 million images each week between different trusts, where their imaging systems otherwise cannot talk to each other. And this is likely to remain a mechanism for the NHS for some time.
But problems including the discovery of data remain, with clinicians often reliant on a patient telling them that a scan has been carried out elsewhere, for the professional to even know to request it from that hospital.
Even then if you have an acute condition that requires instant access to images, sometimes the quickest and most clinically beneficial thing to do is to repeat the scan.
Regional shared imaging data
Regional approaches to medical imaging in the NHS are starting to overcome the obstacle. Trust collaboratives, like those seen in Greater Manchester and the SWASH consortium on the south coast of England, have started to enable more seamless access to imaging across their footprint.
By consolidating technology across the region, imaging is available immediately to the people providing care, regardless of which hospital they work in, or where in the consortium the patient’s images were acquired from.
These forward thinking regions are making great strides when it comes to delivering faster and better diagnoses, in enabling clinical collaboration and informed decisions, and being able to balance workload and availability of specialists across their region.
But the challenge still remains of making imaging available to professionals who might need access outside of their region – for example if a particular specialist works elsewhere, or if a patient moves to another location for treatment.
Standards in imaging
One of the principles set out in the draft data strategy is a vision for the data architecture that underpins health and care to make it easier for better use of data no matter where it is kept. And that in part rests on standards – with a commitment for “clear and open standards” to drive interoperability.
This is one area that the imaging technology community needs to pay close attention to. Not surprisingly, the strategy doesn’t delve into the required standards for imaging – that’s not its purpose.
But developing stronger standards in the imaging environment, in keeping with the principles of the strategy, could enable much better access to important data if those standards were consistently adopted.
Standards such as DICOM, XDS, XDSi, XCA, and WADO – to name a few, do already exist in imaging. Some of these standards are already being used to allow imaging to be pulled or viewed across different IT systems and from one region to another.
The challenge is that two vendors incumbent in two different regions may have different interpretations of the same standard. And so if different regions want to make imaging seamlessly available to each other, a significant amount of integration work may be required.
The opportunity is for vendors and others working in imaging to think about how they might better align with the principles in the new strategy. Industry needs to work together to establish and develop those standards to a level of maturity where we don’t have such varied interpretation. There are several influential groups making great strides in this area, however, it is a complex topic so progress can be slow, meaning that the reality of true, extra-regional ‘plug and play’ interoperability may be some way off.
The radiology domain is the most mature in terms of standards adoption than any of the other diagnostic disciplines. However, even today, there are examples of radiology implementations that are not utilising DICOM as their storage standard. This can be an inhibitor to future progress so a responsibility lies with the procurement function to demand IT systems that are fully conversive with these standards – DICOM has been recognised as an international standard for medical imaging since 1993.
Taking a more robust approach to standards could lead to a situation where a clinician could query a database for imaging on an individual that might have been captured anywhere in the country.
Could NHSX go further on medical imaging?
NHSX’s strategy does contain a number of direct references to innovation in the imaging space resulting from improved data availability. For example, it describes how AI innovators have “real potential to improve the delivery of health and care services by analysing large quantities of complex information”. This includes reference to several imaging AI developers.
It details the value of the National COVID-19 Chest Imaging Database – a centralised UK database containing x-ray, CT and MRI images from patients across the country. The database is intended as a means for researchers to better analyse and understand the impact of COVID-19 and as a resource for developers to train AI tools.
And, in a section on its commitment to separating the data layer from the application layer – where data is stored in a more accessible point in the cloud rather than being locked-in with vendors – reference is made to the procurement of new laboratory information management systems (LIMS) and radiological information systems (RIS).
But NHSX could go further in its thinking on imaging. Just taking this last idea, though separating data from a LIMS or RIS may make sense, this approach could be valuably applied to other departmental systems, including imaging systems like the picture archiving and communication system (PACS).
LIMS and RIS traditionally contain textual data. But a histopathology study in a PACS regularly exceeds 15GB or more. If NHS trusts were to physically share that data – moving it from one environment to the next could result in exabytes worth of imaging data being duplicated. Hosting that imaging in the cloud could avoid that replication and make the data much more easily accessible at the point of care, and, once anonymised, for research.
Whilst the COVID imaging database is likely to prove highly useful, as NHSX looks to expand this, it might consider the value of imaging access for research on many other diseases.
Imagine if researchers with a legitimate reason could quickly access 200,000 anonymised chest x-rays or MRI scans. This could be an incredible boon to medical research domains, and for the development of many new drugs and treatments that rely heavily on longitudinal data, but which are sometimes hampered by data access.
A welcome strategy
I look forward to seeing the final strategy, following NHSX’s consultation. The strategy has started to advance the agenda in developing a technical layer and a governance layer across silos to make data available to those who need it most in a way that is safe and secure. This is certainly one for the medical imaging sector to take note of.